Mentalhealth in Perimenopause & Menopause (Psychology Connections WA Talk)
- purity carr
- Mar 6, 2024
- 12 min read
Updated: Jun 14, 2024
Connections WA: Counselling, Psychology, Occupational Therapy and Speech, Language and Communication
Port Kennedy
This is from a talk that I delivered at Connections WA on the evening of 6th March 2024.


WHAT CAUSES PMS

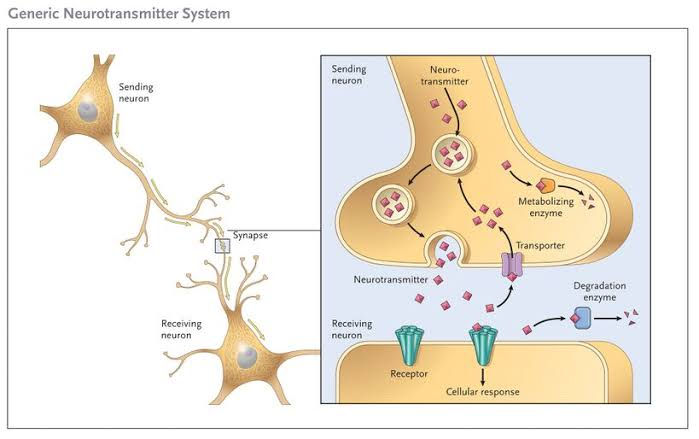
Estrogen and progesterone, two key hormones involved in regulating the menstrual cycle, rise and fall throughout the month. In the days leading up to menstruation, levels of these hormones can fluctuate, sometimes leading to imbalances. These hormonal changes can impact neurotransmitters in the brain, such as serotonin, which plays a key role in mood regulation. Low levels of serotonin are associated with feelings of irritability, mood swings, and anxiety, which are common symptoms of PMS.
In addition to hormonal factors, other factors can contribute to the severity of PMS symptoms. These may include:
1. Stress: High levels of stress can exacerbate PMS symptoms by affecting hormone levels and increasing feelings of anxiety and irritability.
2. Dietary Factors: Poor dietary habits, including excessive consumption of caffeine, sugar, and salt, can worsen PMS symptoms. Certain nutritional deficiencies, such as low levels of magnesium or vitamin B6, may also play a role.
3. Lifestyle Factors: Lack of exercise, inadequate sleep, and unhealthy lifestyle habits can all contribute to the severity of PMS symptoms.
4. Psychological Factors: Women who have a history of depression or other mood disorders may be more susceptible to experiencing severe PMS symptoms.

What can psychologists and counsellors do to help women manage PMS?
Counselors and psychologists can offer valuable support to women experiencing premenstrual syndrome (PMS) by providing various therapeutic interventions tailored to their individual needs. Here are some ways in which counselors and psychologists can help:
1. Psychoeducation: Counselors can educate women about PMS, its symptoms, and its underlying causes. Understanding the biological and psychological factors contributing to PMS can help women feel more empowered and less overwhelmed by their symptoms.
2. Cognitive Behavioral Therapy (CBT): CBT is a type of therapy that focuses on identifying and challenging negative thought patterns and behaviors. Counselors can teach women coping strategies and relaxation techniques to manage stress and regulate emotions during the premenstrual phase.
3. Mindfulness and Relaxation Techniques: Psychologists may teach mindfulness-based techniques, such as meditation, deep breathing exercises, or progressive muscle relaxation, to help women reduce anxiety, improve mood, and enhance overall well-being.
4. Stress Management: Counselors can work with women to identify sources of stress in their lives and develop coping strategies to better manage stressors, which can help alleviate PMS symptoms.
5. Supportive Counseling: Providing a safe and supportive space for women to express their feelings and concerns about PMS can be immensely beneficial. Counselors can offer empathy, validation, and nonjudgmental support, helping women feel understood and less alone in their experiences.
6. Lifestyle Modifications: Psychologists may assist women in making lifestyle changes that can alleviate PMS symptoms, such as improving diet and nutrition, promoting regular exercise, optimizing sleep habits, and reducing caffeine and alcohol consumption.
7. Medication Management: In some cases, psychologists may collaborate with medical providers to explore medication options for managing severe PMS symptoms, hormonal therapies. Contraceptions are synthetic, they work for contraception but they are not biologically active, this means that women experience associated mood symptoms with contraception without helping PMS.
Toping up hormones with "natural hormones" body identical HRT can be useful in helping smooth the estrogen fall curve.
THIS IS HOW CONTRACEPTIONS CAN LOWER TESTOSTERONE LEVELS WHICH CAN LEAD TO LOW LIBIDO, BRAIN FOG, LACK OF ENERGY & VITALITY, ACHES & PAINS
The mechanism by which hormonal contraceptives may lower testosterone levels primarily involves the suppression of the body's natural hormone production and hormonal feedback loops.
Suppression of ovarian function: Hormonal contraceptives typically contain synthetic forms of estrogen and/or progestin. These synthetic hormones work by suppressing the normal hormonal fluctuations that occur during the menstrual cycle, including the suppression of ovulation. By preventing ovulation, hormonal contraceptives reduce the production of ovarian hormones, including testosterone, which is produced in small amounts by the ovaries.
Feedback inhibition: Synthetic hormones in contraceptives can also disrupt the feedback mechanisms that regulate hormone production in the body. For example, elevated levels of estrogen and progestin from hormonal contraceptives can signal to the brain (specifically the pituitary gland) that there is enough hormone in the system, leading to a decrease in the production of gonadotropin-releasing hormone (GnRH) and luteinizing hormone (LH). LH is necessary for the production of testosterone in the ovaries and adrenal glands. Therefore, decreased LH levels can result in lower testosterone production.
Direct effects on androgen receptors: Some synthetic progestins used in hormonal contraceptives may have anti-androgenic properties, meaning they can compete with testosterone for binding to androgen receptors in the body. This competition may further reduce the biological effects of testosterone.
Is PMS same as PMD or PMDD?
Premenstrual syndrome (PMS), premenstrual dysphoric disorder (PMDD), and premenstrual exacerbation (PME) are related conditions, but they differ in terms of severity and diagnostic criteria:
1. Premenstrual Syndrome (PMS): PMS refers to a collection of physical and emotional symptoms that many women experience in the days leading up to menstruation. These symptoms can include mood swings, irritability, bloating, breast tenderness, fatigue, and changes in appetite. PMS is relatively common and may cause discomfort or mild impairment in daily functioning, but it typically does not severely impact a woman's quality of life.
2. Premenstrual Dysphoric Disorder (PMDD): PMDD is a more severe form of premenstrual syndrome characterized by debilitating emotional and physical symptoms that significantly interfere with a woman's daily life and functioning. The symptoms of PMDD are similar to those of PMS but are much more severe and may include extreme mood swings, severe depression, irritability, anxiety, and tension. PMDD can significantly impair a woman's ability to carry out her daily activities, maintain relationships, and fulfill responsibilities at work or school.
3. Premenstrual Exacerbation (PME): PME refers to the worsening of existing psychiatric disorders, such as depression, anxiety, or bipolar disorder, in the premenstrual phase of the menstrual cycle. Women with PME experience exacerbation of their psychiatric symptoms during the premenstrual period, which can significantly impact their overall mental health and well-being.
While PMS is considered a milder condition that affects many women to some degree, PMDD and PME are more severe and may require specialized treatment, including medication and psychotherapy, to alleviate symptoms and improve quality of life. It's essential for women experiencing significant distress or impairment due to premenstrual symptoms to seek support from healthcare professionals for accurate diagnosis and appropriate management.
WHAT ABOUT TREATMENT FOR BIPOLAR AND DEPRESSION WITH PSYCHOSIS WITH ANTIPSYCHOTICS?
Antipsychotic medications can potentially affect estrogen levels, although the exact mechanisms and effects can vary depending on the specific medication and individual factors. Some antipsychotics, particularly older typical antipsychotics, may have side effects that can impact hormone levels, including changes in estrogen. Examples are Quetiapine (Seroquel), Aripiprazole, Olanzapine, Resperadone, Haloperidol, Clozapine.

One mechanism by which antipsychotics may affect estrogen levels is through their influence on the hypothalamus-pituitary-gonadal (HPG) axis, which regulates the production and release of sex hormones, including estrogen. Antipsychotics can interact with dopamine receptors in the brain, which in turn can affect the release of gonadotropin-releasing hormone (GnRH) from the hypothalamus. Changes in GnRH secretion can subsequently impact the secretion of luteinizing hormone (LH) and follicle-stimulating hormone (FSH) from the pituitary gland, which are essential for regulating ovarian function and estrogen production.
Additionally, some antipsychotic medications may directly influence estrogen metabolism or clearance in the body, potentially leading to alterations in estrogen levels. However, the specific effects can vary depending on factors such as the individual's metabolism, dosage of the medication, and duration of treatment.
Estrogen and testosterone can be effective in treating menopause-related depression for several reasons:
1. Neurotransmitter Regulation: Estrogen and testosterone play essential roles in regulating neurotransmitters in the brain, including serotonin, dopamine, and norepinephrine. Imbalances in these neurotransmitters are associated with depression, and hormonal fluctuations during menopause can contribute to mood changes. Estrogen and testosterone supplementation can help restore balance to these neurotransmitter systems, alleviating depressive symptoms.
2. Neuroprotective Effects: Estrogen has neuroprotective properties that can help maintain cognitive function and protect against age-related cognitive decline. It also promotes neuroplasticity, which is the brain's ability to adapt and reorganize neural pathways in response to experiences and environmental changes. These neuroprotective effects may contribute to improvements in mood and overall well-being during menopause.
3. Impact on Mood and Energy Levels: Both estrogen and testosterone can influence mood and energy levels. Estrogen has been shown to improve mood, reduce irritability, and increase feelings of well-being. Testosterone supplementation in women can also improve mood, energy, and motivation, particularly in those experiencing symptoms of low libido and fatigue associated with menopause.
4. Management of Vasomotor Symptoms: Menopausal symptoms such as hot flashes and night sweats can significantly impact mood and quality of life. Estrogen therapy is effective in reducing the frequency and severity of vasomotor symptoms, which can indirectly improve mood and reduce depressive symptoms.
5. Bone and Muscle Health: Testosterone plays a role in maintaining bone density and muscle mass, which can decline during menopause. Improvements in bone and muscle health can contribute to overall well-being and may indirectly alleviate depressive symptoms by increasing physical strength and mobility.
It's important to note that hormone therapy should be prescribed and monitored by a healthcare provider, as individual hormone levels and medical history can vary. Additionally, the risks and benefits of hormone therapy should be carefully considered, particularly in women with a history of hormone-sensitive cancers or other medical conditions.
What about ADHD
The genetics of ADHD is complex, and while researchers have identified several genes that may be associated with the disorder, there is no definitive list of specific genes responsible for ADHD. Instead, ADHD is believed to be influenced by several genes, each contributing a small effect to the overall risk of developing the disorder.
Research into the genetics of ADHD has identified candidate genes involved in neurotransmitter pathways, brain development, and regulation of attention and impulse control. Some of the genes that have been studied in relation to ADHD include:
1. Dopamine-related genes: Genes involved in the dopamine neurotransmitter system, such as DRD4 (dopamine receptor D4) and DRD5 (dopamine receptor D5), have been implicated in ADHD. Variations in these genes may affect dopamine signaling in the brain, which is thought to play a role in attention and reward processing.
2. Serotonin-related genes: Genes involved in the serotonin neurotransmitter system, such as SLC6A4 (serotonin transporter gene), have also been studied in relation to ADHD. Serotonin is involved in mood regulation, impulse control, and cognitive function, and variations in serotonin-related genes may contribute to ADHD symptoms.
3. Neurodevelopmental genes: Genes involved in brain development and neuronal connectivity, such as BDNF (brain-derived neurotrophic factor) and SNAP25 (synaptosomal-associated protein 25), have been implicated in ADHD. These genes play roles in neuronal growth, synaptic plasticity, and neurotransmitter release, which are essential for normal brain function.
4. Other candidate genes: Additional genes implicated in ADHD include those involved in the regulation of glutamate neurotransmission, such as GRIN2A (glutamate receptor, ionotropic, N-methyl-D-aspartate 2A), as well as genes involved in the circadian rhythm and sleep regulation.
It's important to note that while variations in these genes have been associated with ADHD in some studies, the genetic basis of ADHD is still not fully understood. The interplay between genetic factors, environmental influences, and other biological and psychological factors likely contributes to the development and expression of ADHD.
Furthermore, genetic research in ADHD is ongoing, and advances in techniques such as genome-wide association studies (GWAS) may help identify additional genes and genetic pathways involved in the disorder in the future.
WHAT IS ADHD
Attention-deficit/hyperactivity disorder (ADHD) is a neurodevelopmental disorder characterized by symptoms of inattention, impulsivity, and hyperactivity that interfere with daily functioning. Treatment options for ADHD typically include a combination of behavioral interventions, medication, and support strategies. Additionally, there is evidence of a genetic component to ADHD, with genetics playing a significant role in the development and expression of the disorder. ADD (Attention Deficit Disorder) is an outdated term that was once used to describe a subtype of ADHD characterized primarily by symptoms of inattention without hyperactivity
1. Behavioral Interventions: Behavioral interventions are often the first-line treatment for ADHD. These may include behavior modification techniques, such as positive reinforcement, time management strategies, organizational skills training, and parent training programs. Behavioral therapy aims to help individuals with ADHD develop coping skills, improve self-regulation, and manage their symptoms more effectively.
2. Medication: Medication is commonly used to manage symptoms of ADHD, particularly in individuals who have moderate to severe symptoms that significantly impact daily functioning. The most commonly prescribed medications for ADHD are stimulants, such as methylphenidate (e.g., Ritalin) and Dexamphetamines These medications work by increasing levels of neurotransmitters like dopamine and norepinephrine in the brain, which helps improve attention, focus, and impulse control. Non-stimulant medications, such as atomoxetine (Strattera) and guanfacine (Intuniv), may also be prescribed, especially for individuals who do not respond well to stimulants or who experience significant side effects.
3. Supportive Strategies: In addition to behavioral interventions and medication, individuals with ADHD may benefit from supportive strategies to address specific challenges associated with the disorder. This may include accommodations at school or work, such as extended time on tests, preferential seating, or assistive technology. Psychoeducation and support groups can also be valuable for individuals with ADHD and their families, providing information, resources, and peer support.
4. Genetic Link: Research suggests that genetics play a significant role in the development of ADHD, with heritability estimates ranging from 70% to 80%. Studies have identified several genetic variants associated with ADHD, particularly those related to dopamine and serotonin neurotransmission, as well as genes involved in brain development and function. However, ADHD is a complex disorder influenced by multiple genetic and environmental factors, and no single gene or genetic mutation can fully account for its development.
Overall, treatment for ADHD is tailored to the individual's specific needs and may involve a combination of behavioral interventions, medication, and supportive strategies. Genetic factors play a significant role in the development of ADHD, but treatment outcomes are influenced by a variety of factors, including environmental influences, comorbid conditions, and individual differences in symptom presentation. Therefore, a comprehensive and individualized approach to treatment is essential for effectively managing ADHD.
How does estrogen and testosterone work in synergy with ADHD medication
Estrogen and testosterone may interact with ADHD medication in several ways, potentially influencing treatment outcomes and symptom management. However, the specific effects of estrogen and testosterone on ADHD medication can vary depending on individual factors, including hormone levels, medication dosage, and overall health. Here are some ways in which estrogen and testosterone may work in synergy with ADHD medication:
1. Hormone Modulation: Estrogen and testosterone can influence the neurotransmitter systems targeted by ADHD medications, such as dopamine and norepinephrine. By modulating hormone levels, estrogen and testosterone may enhance the effects of ADHD medication on neurotransmission, leading to improvements in attention, focus, and impulse control.
2. Cognitive Enhancement: Estrogen and testosterone have been shown to have cognitive-enhancing effects, including improvements in memory, attention, and executive function. When combined with ADHD medication, which also targets cognitive function, estrogen and testosterone may synergistically enhance cognitive performance and reduce ADHD symptoms.
3. Mood Regulation: Hormonal fluctuations during the menstrual cycle or menopause can impact mood and emotional regulation, which may exacerbate ADHD symptoms in some individuals. Estrogen and testosterone supplementation may help stabilize mood and reduce emotional lability, complementing the mood-stabilizing effects of certain ADHD medications.
4. Sex Differences: ADHD often presents differently in males and females, with females typically exhibiting more internalizing symptoms and males more externalizing symptoms. Estrogen and testosterone may play a role in modulating these sex differences and influencing the response to ADHD medication based on gender-specific hormonal profiles.
5. Comorbidity Management: ADHD frequently co-occurs with other psychiatric disorders, such as depression, anxiety, and bipolar disorder, which exercebate ADHD symptoms.
DIFFERENCE BETWEEN WOMEN, GIRLS AND MALE SYMPTOMS PRESENTATION Internalizing and externalizing symptoms of ADHD
The differences between internalizing and externalizing symptoms of ADHD in women are primarily related to how the symptoms manifest and are expressed.
Internalizing symptoms:
Internalizing symptoms typically involve behaviors that are directed inwardly and may not be as obvious to others.
In women with ADHD, internalizing symptoms may include feelings of low self-esteem, self-doubt, excessive worry or anxiety, depression, and difficulty managing emotions. These symptoms are often experienced internally and may not be readily apparent to those around them.
Women with ADHD may also internalize their difficulties with attention and organization, leading to feelings of frustration, inadequacy, and a sense of being overwhelmed.
Internalizing symptoms may contribute to issues such as perfectionism, social withdrawal, and difficulty seeking help or support.
Externalizing symptoms:
Externalizing symptoms are more outwardly observable behaviors that affect interactions with others and the environment.
In ADHD, externalizing symptoms often include hyperactivity, impulsivity, and disruptive behaviour. However, these symptoms may present differently in women compared to men.
Women with ADHD may exhibit fewer overtly disruptive behaviors commonly associated with ADHD, such as hyperactive and impulsive actions. Instead, they may display more subtle externalizing symptoms, such as difficulty maintaining focus in conversations, interrupting others, or being disorganized in their daily lives.
Externalizing symptoms in women with ADHD may also include difficulty managing time, impulsively starting multiple tasks without completing them, and challenges with executive functions such as planning and organization.

Testosterone And women's well-being
Testosterone is often associated with male reproductive health, but it also plays important roles in women’s bodies. In women, testosterone is primarily produced by the ovaries and adrenal glands, although smaller amounts are also produced by other tissues such as fat cells and skin. Testosterone contributes to various physiological processes and functions in women, beyond just libido. Here are some of the key roles of testosterone in women:
1. Sexual Health: While testosterone is commonly associated with libido (sexual desire) in both men and women, it also plays a role in sexual arousal and satisfaction. Adequate testosterone levels are important for maintaining healthy sexual function and may contribute to overall sexual well-being in women.
2. Bone Health: Testosterone helps maintain bone density and strength, which is crucial for preventing osteoporosis and reducing the risk of fractures, especially after menopause when estrogen levels decline. Testosterone supplementation may be beneficial for women with low testosterone levels who are at risk of osteoporosis.
3. Muscle Mass and Strength: Testosterone contributes to the development and maintenance of lean muscle mass and strength in women. Higher testosterone levels may promote muscle growth and improve physical performance, which can be beneficial for overall health and fitness.
4. Energy and Vitality: Testosterone is thought to play a role in energy levels, vitality, and overall well-being. Women with low testosterone levels may experience symptoms such as fatigue, reduced stamina, and decreased motivation, which can negatively impact quality of life.
5. Cognitive Function: Testosterone receptors are present in various areas of the brain, and testosterone may influence cognitive function, including memory, spatial ability, and attention. Some research suggests that testosterone supplementation may have cognitive-enhancing effects in women, although more studies are needed to fully understand its role.
6. Mood Regulation: Testosterone may play a role in mood regulation and emotional well-being in women. Low testosterone levels have been associated with symptoms of depression, anxiety, and irritability, while testosterone supplementation may improve mood and emotional stability in some individuals.
INTERMITTENT FASTING RESOURCES CAN HELP WOMEN UNSTICK STUBBORN WEIGHT

Dr Purity Carr
GP & Menopause Doctor
Harvey, WA, #drpuritycarr






Comments